What is cancer?
Cancer is a disease where the regulation of cells in our body goes haywire. Instead of normally growing, functioning, staying in their locations and eventually dying, cancer cells stop behaving normally. Cancer is not a single disease but rather an overall term we apply to these types of diseases. Unlike bacteria or viruses which our bodies can see as “foreign” and attack using our immune responses, cancer is more difficult because cancer arises from cells within our bodies. Our bodies may not see cancer as foreign even though those cells are no longer working as they should.
Dr. Phil Gold.
While working in the Montréal General Hospital in the 1960s, Dr. Phil Gold saw many patients with cancer, who had undergone surgery to remove tumors and after their surgeries the patients had treatment with either radiation or with anti-cancer drugs (chemotherapy). The radiation and drug treatments at that time targeted cells that divide quickly, which is a feature of cancer cells. Unfortunately, other cells in the body, such as hair, skin, blood cells and cells lining the gut, also replicate quickly which leads to their destruction along with the cancer cells. Patients suffered horrible side effects from the treatments and Dr. Gold asked himself, “is there nothing more specific about cancer cells that could be used as targets for therapy?” He had read a science journal article that reported there was no marker yet for cancer and concluded that “nor would one ever be found”. He disagreed and thought he should look for one.
The field of Immunology was exploding at that time, so Dr. Gold turned to immunology for the tools to help him in his search. One such immunological tool was antisera, the material in the blood that contains antibodies. Animals could be injected with tumor material then their blood collected and the antitumor antisera isolated from the blood. As there were no cancer markers at that time, it was difficult to isolate and separate tumor material from non-cancer or normal material. Dr. Gold needed a way to be certain that the antibodies made when he injected the material into the animals were specific to the cancer cells and not normal cells.
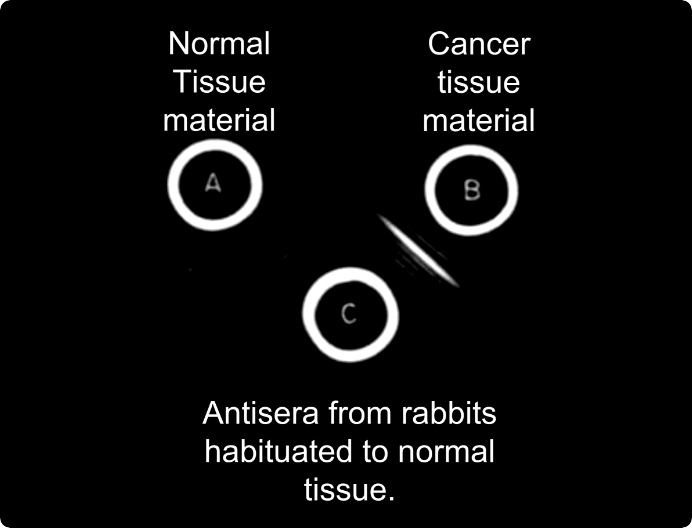
Antisera of rabbit habituated to normal tissue (C) reacts with the colorectal cancer material (B)
but not with the normal tissue material (A), as shown by a bright white band
Researchers had shown that it was possible to make animals “acquired immune tolerant”. They exposed mice of one strain (for example, Strain A) shortly after birth to cells from mice of a different strain (Strain B), and then later when the Strain A become adults, the scientists saw that the Strain A mice did not make antibodies to tissue from Strain B mice. In other words, the immune responses of strain A mice recognized cells of strain B mice to be like themselves rather than to be foreign. Dr. Gold wanted to try a similar experiment but instead of using different strains of mice, he would use different species of animals. He wanted to see whether exposing baby rabbits to human tissue could make the baby rabbits “immune tolerant” to the normal human tissue. Dr. Gold had a saying “when you are looking for a needle in a haystack, the first step is to remove the haystack”, and searching for a cancer biomarker was definitely a needle in the haystack. His plan to make the rabbits immune tolerant to the normal tissue was his way of removing the “haystack” or any antibodies that would be generated to normal tissue. Later, when the rabbits became older and he gave them injections of tumor tissue, the animals should make antibodies only to the cancer particles.
Next, Dr. Gold needed to find tumor and non-tumor material that came from the same patient. At that time, tissues from the surgeries came either from patients with cancer, or for the non-cancer material, patients who were getting surgeries for non-cancer reasons. He wanted to avoid the complications that any immune responses made would have been in response to the material coming from different people, rather than between tumor and non-tumor material. In his reading of scientific papers, he found that tumors in the bowel of colonic cancers do not spread more than 5-6 cm in size from the tumor as visible to the eye, and that typically the surgeons, when removing the tumors, would cut out areas slightly larger beyond the tumor. Dr. Gold now had material from the same patient that he could confidently separate into tumor tissue and normal tissue and he prepared these materials for injection into the animals.
A second challenge arose in making the “acquired immune tolerant” baby rabbits. Mother rabbits do not like their babies to be handled by strangers. The scent of a stranger on the newborn rabbits could lead the mothers to harm and even kill their offspring. Dr. Gold had to get the mother rabbits used to his scent, so he spent long periods of time in the animal rooms with the mother rabbits before they gave birth. The mother rabbits got used to his smell while, Dr. Gold found his colleagues were avoiding him in the coffee lounge. Within 8 hours of their birth, Dr. Gold gave the newborn rabbits their first injection with non-tumor material (normal material) from patients. Later, when these rabbits became adults and were immune tolerant to normal human bowel material, he then injected them with cancer tissue from the same patient whose normal bowel tissue they had received shortly after their birth. Weeks later he collected antisera from these rabbits.
Dr. Gold then tested the antisera in an assay where in an agar gel (similar to Jell-o but you don’t eat it) there was a central well into which he would put the tumor material and in surrounding wells, he placed the different antisera. The materials in the wells would seep into the gel and if the antisera reacted to the tissue material being testing, a banding pattern would slowly appear. As these banding patterns took time to develop, he brought the plate home for the weekend. The next day, after their morning coffee, both he and his wife looked at the plates and saw a single white band in the gel: there was a reaction between the tumor material and the antisera from the immunologic tolerant rabbits that had later been injected with tumor material. The baby rabbits’ immune systems had treated the normal tissue as ‘self’ and had generated antibodies against something in the tumor material. Finally, here was the evidence that the tumor material contained something unique that was not found in the normal material. At that moment, Dr. Gold realized he knew something that no one else in the world knew. He had identified a cancer marker. On Monday, he quickly told everyone in the laboratory. In 1965, he and his supervisor, Dr. Samuel Freedman, published this groundbreaking research of the first report of a cancer-specific marker in the Journal of Experimental Medicine.
He presented his research at the Physiology Department of McGill where he was asked whether this cancer molecule could also be found on embryos during development. Dr. Gold tested and found that the antisera reacted with gut, liver and pancreas tissue from the embryonic material. The molecule to which the antisera reacted was then named carcinoembryonic antigen (CEA) to reflect both its cancer and embryonic expressions.
Next, Dr. Gold and his colleagues devised an assay where they were able to detect a billionth of a gram of CEA in one milliliter of human plasma. They published this method in 1969 and this groundbreaking assay, the first time one could test human blood for a cancer biomarker, was initially met with silence. The cancer research community was skeptical of new findings as many research reports were not reproducible. To help convince the science community, Dr. Gold offered to ship the antisera to various research labs around the world so they could test it on their own samples. Once these different groups were able to see the antisera working in their own hands, and on their own samples, there was an overwhelming positive reaction to his findings and this began his collaborative work with many different research groups.
In 1972, the CEA assay was the first detection method of cancer that was approved for sale. Today, CEA detection continues to be used as a means of monitoring those patients with cancer.
.jpg)
Dr. Clifford P. Stanners
Prof. Cliff Stanners always wanted to become a scientist whereas his mother had dreams of him becoming a medical doctor. He decided to compromise and he went into medical research. Prof. Stanners studied and researched at the Ontario Cancer Institute (O.C.I.) at the Princess Margaret Hospital in Toronto. He often found himself riding the elevators with cancer patients and he would talk with them and their families. From his conversations, he had a direct understanding of the difficulty the anti-cancer treatments had on the patients. To this day, he thinks that his understanding of cancer is one of his scientific strengths, along with his knowledge of cell biology and molecular biology.
In 1982 Prof. Stanners joined McGill’s Department of Biochemistry and later became the director of the McGill Cancer Center in 1988, a position he held until 2000.
Prof. Stanners thought the CEA story was very exciting. Prof. Gold had been able to identify CEA because it was expressed at high levels on cancer cells. CEA was highly expressed in approximately 70% of human cancers, however, it turned out that it was also expressed, generally at lower levels, on normal cells. As a cell biologist, he found this very interesting, and he wanted to understand its function in normal cells and why it was so closely associated with tumor transformation.
One of the first steps to take after identifying a new marker is to clone the gene for the marker, which helps the scientists to better study the gene, and its function and understand how its expression is controlled. In 1987, Prof. Nicole Beauchemin, who at the time was a post-doctoral fellow in Prof. Stanners’ lab, published the DNA sequence of the full-length cloned gene.
Soon after, in 1989, Prof. Stanners’ team including Prof. Beauchemin, showed the function of CEA was as an adhesion molecule. Adhesion molecules are needed in the body so cells can attach to each other, to fix cells to a specific location in tissue by binding to the extracellular matrix, and control the movement of cells. Adhesion molecules can also function as translators, in that they convey information from the extracellular matrix and outside the cell, then activate signaling pathways inside the cells that can lead to specific cell responses.
Around this time, researchers, both at the Goodman Cancer Institute and in laboratories around the world, after cloning CEA found that there were other molecules that shared features similar to those of CEA; a family of CEA molecules. These family members had shared common structural elements but also differed in other ways. In 1999, it was agreed to name the members of this gene family as “carcinoembryonic antigen cell adhesion molecules” or CEACAM. The original CEA identified by Prof. Gold was then recognized as CEACAM5.
Prof. Stanners showed that the members of the CEACAM gene family are distributed on the cell surface membrane in clusters, termed“rafts” and that CEA could attach (bind) to many different molecules: it could bind with itself, other CEACAMs, or other adhesion molecules such as integrins or proteins. Through blocking different sections of the CEACAM molecules he could see whether their ability to attach to other adhesion molecules was affected, and then he would determine whether subsequent events occurred or not. By this process, he was able to identify the different signaling pathways that were activated in response to the CEACAMs.
To study the function of molecules, both in the normal body and in a diseased state, scientists rely on animal models, such as mice. In the case of CEA, however, mice do not possess the mouse version of CEA, but they do express other types similar to human CEACAM1 and 2. As it is difficult to use wild-type mice to assess the effects of the other CEACAM members, decades of research have been performed using cells in culture (in vitro), and later, mice modified to express human CEACAMs (transgenic mice).
Cancer is a multi-step process in which normal cell behavior goes awry. These steps include cells growing and replicating (proliferating) without limits, cells not maturing or differentiating, cells changing to an incorrect shape (morphology), cells evading a programmed cell death (apoptosis) and eventually, cells leaving their local region and moving to other places in the body (metastasis).
Prof. Stanners spent decades painstakingly researching how CEA and its family of CEACAMs are involved in the multi-step process of cancer. Using rat myoblast cells, which should normally mature into muscle cells, he showed that by expressing human CEA in these cells, the maturation or differentiation process would be stopped. He and his team showed that when they took human colonic cells, and manipulated them to overexpress CEA and CEACAM6 at levels 10- to 30-fold higher than normal, which were the levels seen in colon cancers, that the cells did not differentiate nor did they form “crypts” which were the normal physical structure or architecture of the colon.
Although much work involved studying the effects of the CEA gene family was performed with cells in culture, there is always a need to observe what happens in complete living creatures (in vivo). Other researchers were successful in generating a mouse expressing human CEA (CEACAM5). Those mice, although expressing CEACAM5 in tissue to the same levels as in human, did not develop tumors. As these mice expressed only human CEA and not human CEACAM6, which in humans are typically expressed together, it was suggested that perhaps both genes were needed in order to see any changes.
Prof. Stanners and his team set out test this idea and they generated transgenic mice by taking a very long stretch of 187 kilobases of DNA, that contained 4 linked genes of human CEA: CEACAM5/CEACAM6/CEACAM3 and CEACAM7. Carlos Chan, a PhD student of Prof. Stanners at that time, was the one who managed to take this long DNA strand or as described by Prof. Stanners, “wrangle a piece of spaghetti 20 feet long without breaking it” into the bacterial artificial chromosome. By this method, they were successful in generating transgenic mice that had either 2 or 10 copies of the transgene. By breeding animals that had 10 copies, they obtained mice with 20 copies.
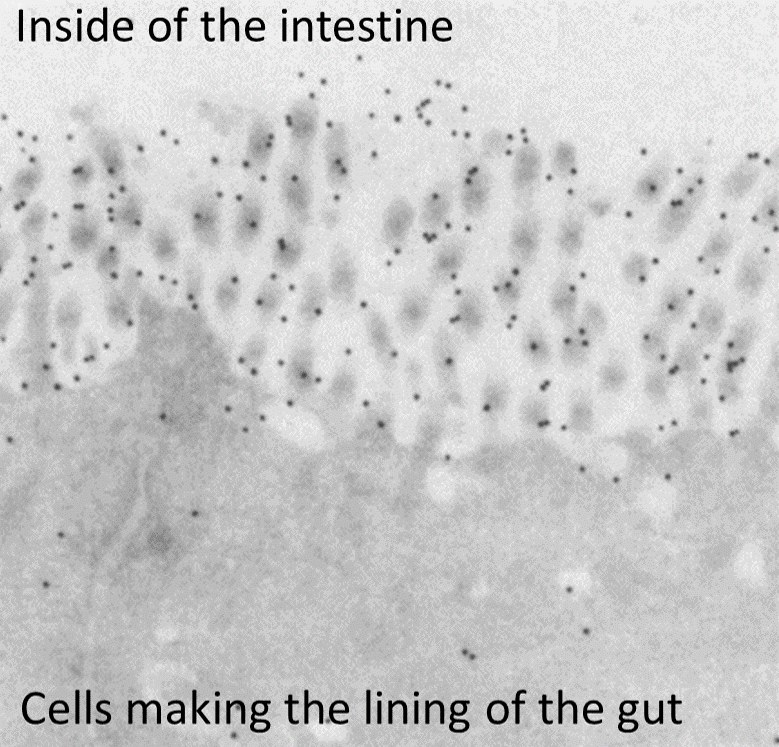
Electron micrograph of the lining of the gut showing CEA (black dots) as adhesion cells residing at the extremities of the cells that make up the lining of the gut.
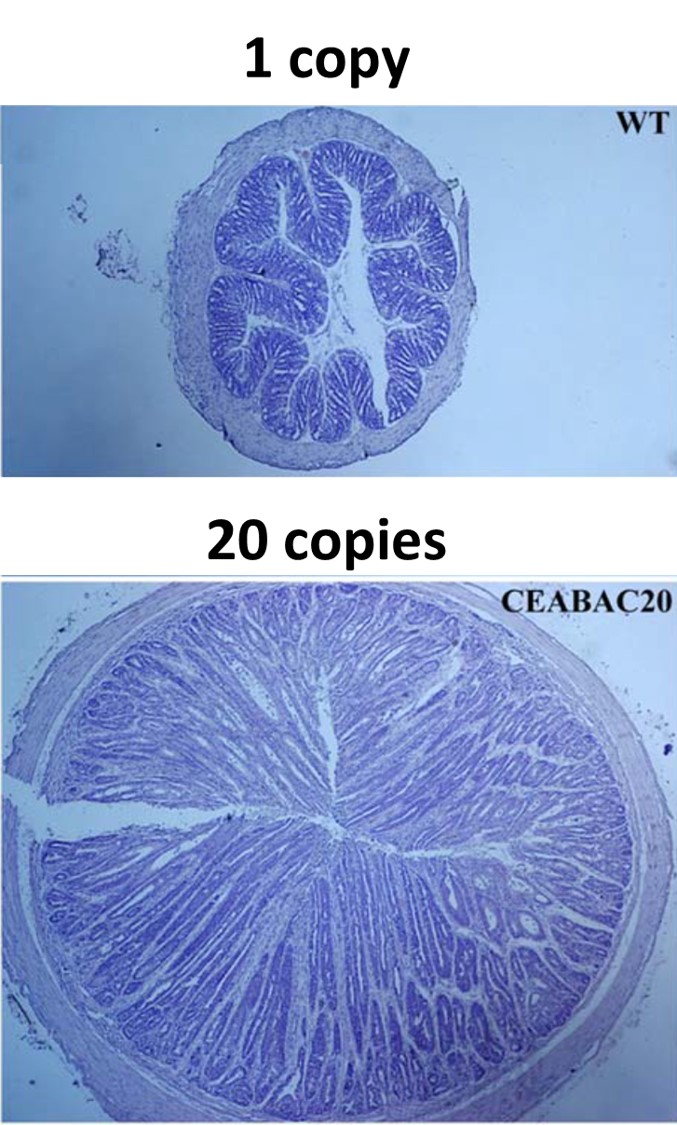
Cross-sections of a mice colons, comparing wild-type mice with transgenic mice in which 20 copies of the human CEA/CEACAM6 was inserted. Mice with 20 copies of the gene develop large colons due to excessive cell proliferation.
An advantage of having mice with 2, 10 and 20 copy numbers of the human CEA/CEACAM6, was that with increasing copy numbers, the researchers saw increasing levels of expression. Any changes between the groups of mice could be attributed to increased gene expression. In the 2-copy mice, the researchers saw little changes as compared to wild-type mice. In contrast, with the 20-copy mice, the researchers immediately saw that the transgenic mice were physically smaller than the wild-type mice. In studying these 20-copy mice, they saw that they expressed high levels of CEA similar to the levels typically found in human colorectal cancers. Although physically smaller in body size, when the researchers looked at the colons of the 20-copy mice, the colons were larger, both in length and in diameter, than those of wild-type mice.
Researchers looked at the colons of the 20-copy mice under the microscope and saw the colon architecture was abnormal and appeared similar to those seen in human colorectal tumors. It is important for the body to maintain the correct architecture of our tissues and organs, therefore the body has the ability to remove any cells that no longer attach to the extracellular matrix by instructing those cells to self-destruct, or die. In the colon of the 20-copy mice, the researchers saw cells that were not properly anchored to the extracellular matrix yet were not dying, indicating that normal control mechanism was not working. The researchers concluded that the reason the 20-copy mice were physically smaller than the wild type mice was that their colons were enlarged because those cells were proliferating too much and not dying when they should, and these abnormal cells meant that the colon architecture was affected, resulting in the colon not able to digest food correctly. In short, the mice were unable to isolate the nutrients they needed from food in order to grow.
A critical finding from his experiments with the 2-, 10- and 20-copy transgenic mice was that Prof. Stanners could argue that decreasing the high expression levels of CEA and CEACAM6 seen in cancer patients down to normal levels could be a way to reduce tumors in humans. Prof. Stanners always wanted to understand human cancer and with the goal of eventually helping patients and his work showed a mechanism to achieve that goal.

Dre Nicole Beauchemin
Prof. Nicole Beauchemin always had an interest in medicine and her original intention was to go to medical school, but after taking a few medical school classes she realized that she preferred to study the causes of disease. Ironically, Prof. Beauchemin ended up teaching McGill medical students for 25 years.
Prof. Beauchemin came to McGill University to work as a post-doctoral fellow in Prof. Stanners’ laboratory, using her molecular biology experience to investigate cancer biomarkers. At the Université de Montréal, for her Ph.D. research, she studied transfer RNA, the molecules that function as the link between messenger RNA and amino acids to form proteins. She recounts being fascinated with multiple aspects of biology, including virology, parasitology, immune systems and even plant science, yet it was in cancer research that she felt she could fulfill her interests. Cancer research could allow her to bridge the basic knowledge of understanding the biology of the disease and hopefully, translate this knowledge into help for cancer patients.
In 1988, Prof. Stanners asked Prof. Beauchemin to join the McGill Cancer Center in the role of Assistant Professor. She was awarded a research grant to observe similarities and differences in mouse models of human cancer biomarkers. Although cancer was her primary focus, Prof. Beauchemin explains that in studying genetically-modified mouse models of human diseases, she had to understand how the genes functioned normally in mice and humans, and then how expression of these genes would change in diseased states. As she was a leader in the field of developing different genetically-modified mouse models, Prof. Beauchemin received numerous requests from fellow scientists for access to her mice. She was always willing to share which enabled her to participate in many different research questions and experiments as a collaborator.
Mice do not have a version of human CEA (CEACAM5) but do express two CEA-related family genes called Ceacam1 and Ceacam2. CEACAM1 is the most widely distributed protein of the CEACAM gene family, and is expressed in many cells such as liver, intestines, kidneys and immune cells including T cells, B cells, neutrophils, macrophages and monocytes. It is also expressed on the epithelial cells of reproductive tissues such as prostate, breast and uterus. Prof. Beauchemin describes CEACAM5 and CEACAM1 acting as mirror images of each other. In a scenario where CEACAM5 would have a positive effect, then CEACAM1 was likely to have a negative effect and vice versa. What will happen in humans if you block CEACAM1, how will the other part of the mirror react?
Prof. Beauchemin wanted to know what would happen in mice if CEACAM1 was not expressed; would the mice survive and if so, what differences could be seen. The Ceacam1 knockout mice did, in fact, survive and when researchers looked at the colons of the Ceacam1 knockout mice, they saw colon cells were proliferating more and cells in the colonic villi were not undergoing the instructed cell-death to the same extent as in wild-type mice. Also, when they treated the animals with a chemical to induce colonic tumors, the Ceacam1 knockout mice had more tumors than wild-type. All this evidence confirmed the idea that CEACAM1 functions as a tumor suppressor.
As CEACAM1 can function as tumor suppressor, Prof. Beauchemin believed it was crucial to understanding how the function of CEACAM1 is controlled. In humans, CEACAM1 can be generated as different isoforms, some of which are secreted, while others are not. Of the non-secreted isoforms, some differ in the extracellular portion of the molecule which is the region involved in the adhesion function of the molecule. Other isoforms differ in lengths of the portions inside the cells, or cytoplasmic domains. These isoforms are aptly named, the long (L) and the short (S) depending on the lengths of their cytoplasmic tails. The signaling experiments performed by Prof. Beauchemin showed that the long form of CEACAM1 (CEACAM1-L), after binding, has residues that are activated, which in turn signal to other molecules to bind to CEACAM1-L and shut down its activation as a way to self-regulate.
As cancer tumors grow in size, they need more oxygen and nutrients. The body has a process to develop new blood vessels, termed “angiogenesis”, which can be helpful to resolve strokes or in some forms of heart disease. Prof. Beauchemin and her team asked whether blood vessels were playing a role in cancer and tumor development. Again, they used the Ceacam1 knockout mice but this time they compared them to mice that were expressing high levels Ceacam1. The researchers wanted to assess how well cells from these different animals were able to grow new blood capillaries. First, they tested whether cells isolated from the animals were able to grow in vitro in a Matrigel. Gels containing cells from the Ceacam1 knockout mice did not have new capillaries whereas gels with cells from the mice overexpressing Ceacam1 had many new capillaries. Next, they looked at the growth of new blood vessel growth in the animals directly, and they showed the CEACAM1 expression was important.
Along with the changes in the colon in the Ceacam1 knockout mice, Prof. Beauchemin and her collaborators observed that Ceacam1 knockout mice were fatter than wild-type mice. To investigate why the animals were fatter they looked at insulin receptor signaling in the liver of the Ceacam1 knockout. In the liver of Ceacam1 knockout mice, insulin clearance is impaired and metabolism of fat is altered, both of which may lead to obesity. Prof. Beauchemin and her colleagues concluded that in the future, when testing CEACAM1 inhibitors as cancer therapy, it may be wise to exclude patients with diabetes or liver disease from the clinical trials or at the minimum, monitor them closely throughout the trials.
One therapy being investigated is the use of immune cells to treat cancer. Prof. Beauchemin studied the effect CEACAM1 has on different types of immune cells. For T cells, CEACAM1 can interact with a T cell protein, TIM-3, which gives it an inhibitory function, ‘calming’ the immune response and limiting inflammation. For B cells, CEACAM1 appears to be involved in B cell maturation and activation. Meanwhile, CEACAM1 expression on tumor cells was shown to play a role in tumors evading the Natural Killer cells. Her works show that CEACAM1 has very different effects on different immune cells, and that it is important to understand these effects, especially if planning on using immune cells as therapy to treat cancers.
With her interest in virology, Prof. Beauchemin began to work with the world’s leading expert on mouse hepatitis virus, a notable coronavirus. As CEACAM1 is an adhesion molecule expressed on many different cell types it is a prime target to be used as a receptor by viruses, both human and mouse pathogens. They showed that Ceacam1 knock out mice could not be infected with the virus, nor develop liver disease, whereas the wild-type mice were infected and developed disease in the liver and spinal cord. These findings showed that CEACAM1 was the sole receptor for this mouse hepatitis virus.
Prof. Beauchemin’s decades of research showed CEACAM1 has activities and functions that are relevant to cancer including proliferation, apoptosis, angiogenesis, inflammation, immune evasion and even modifying cellular energetics (insulin).
As a breast cancer survivor herself, Prof. Beauchemin recounts the effect and impact of the aggressive treatment therapies she had to undergo. She is hopeful that her research can improve cancer treatments to benefit cancer patients.
Summary
The last 50 years of research on the CEACAM gene family have produced findings that demonstrate their important roles in both normal states and in cancer. This profound scientific legacy is a credit to Drs. Gold, Stanners and Beauchemin, to a large number of graduate students and post-doctoral fellows as well clinical collaborators and a large community of scientists sharing the same interests and outlook: understanding the biology that leads to cancer development and metastasis and the identification of novel targets (markers) whereby we may be able to conquer and cure cancer.
Public lecture series
Learn how the Goodman Cancer Institute legacy, through research mentorship, leads to groundbreaking testing and drug discoveries.
Nahum Sonenberg and his scientific contribution to mRNA biology